project04:P2
P2
The Academic Medical Center(AMC) is one of the largest hospitals in the Netherlands. The AMC is among the top medical centers in the world. The building dates back to the eighties of the last century. Up until now various architectural interventions have been made but the currently the quality of the building is right on the acceptable level. To maintain an acceptable quality of the building renovation and transformation is required. Therefor the AMC building has to be renewed to face the future. Designing new state of the art medical facilities as for creating a sustainble hospital with a neutral carbon footprint. Within the Architectural Enigineering graduation track this challenge is explored. This is the second presentation in the graduation track presenting my proposal for the new AMC based on Robotic Building principles.
The future of healthcare and the hospital
The patient, health and healthcare
Survivability is at the core of every human being. Everything we do we do to survive. In order to live longer and survive diseases we have developed a large and complex healthcare system. One of element of this system is the hospital. This place is designed as a last resort, a last chance for the ill to get better. Since the hospital is a place for healing and becoming well, it would imply that being within a hospital would be experienced as a pleasant experience. But on the contrary people often experience anxiety and discomfort.
This is due to that same survivability, it is when we become ill we become uncertain. We lose the control of the situation of health. As a consequence of this uncertainty it becomes difficult to predict what will happen next. Which then can result in feelings like isolation, alienation and depression. These feelings do not improve the potential for regeneration. Patients can suffer from increased blood pressure, stress, reduced sleep.
But this is not what a hospital should cause any patients. It is here where architecture could play a role, a role to prevent these negative emotions from ever occuring and put patients at ease. Research done to find out which design factors matter to patients to create a healing environment. It proposes six themes with associated design characteristics to improve the healing environment; Spatial comfort, Privacy, Autonomy, Sensory comfort, Safety and security, and Social comfort.
Spatial Comfort.
The research describes spatial comfort as a collective term for comfort provide by physical features and use of space in the environment. A space is deemed as comfortable if it is able to support activities a person wants to execute within the space, personal needs, and social interaction.
Privacy.
Privacy is described as the need for one's own territory and the ability to shut out information about others. Privacy is an umbrella term which covers auditory (sound), visual (sight), tactile (touch), spatial (personal space) and olfactory (smell) privacy. This research suggest that several design characteristics affect the perception of privacy all influencing one or more of these umbrella factors.
Autonomy.
Autonomy refers to the freedom to the determination of one's own action and behavior and the experience control. In the current situation patients are dependent on hospital staff and therefor lack control over their treatment. design characteristics are therefor focusing on placing control into patients hands.
Sensory comfort.
The term of sensory comfort collects the factors that provide comfort through the environment on human senses. I describes design factors as daylight, fresh air and scent, e.g. all these should than result in a space that is experienced as pleasant.
Safety and security.
The feeling of safety is influenced by the feelings of prospect, refuge, and escape. Within the hospital context it is associated with overview, lines of sight, storage and observation of staff. The design of hospital rooms should provide these design factors and will than contribute to the well being of the patients.
Social comfort.
This subject refers to the emotional, informative, and instrumental support provided by friends, family, staff and other patients. Social support has shown that it has the potential to improve someones physiological wellbeing. (Schreuder, Lebesque, & Bottenheft, 2016)
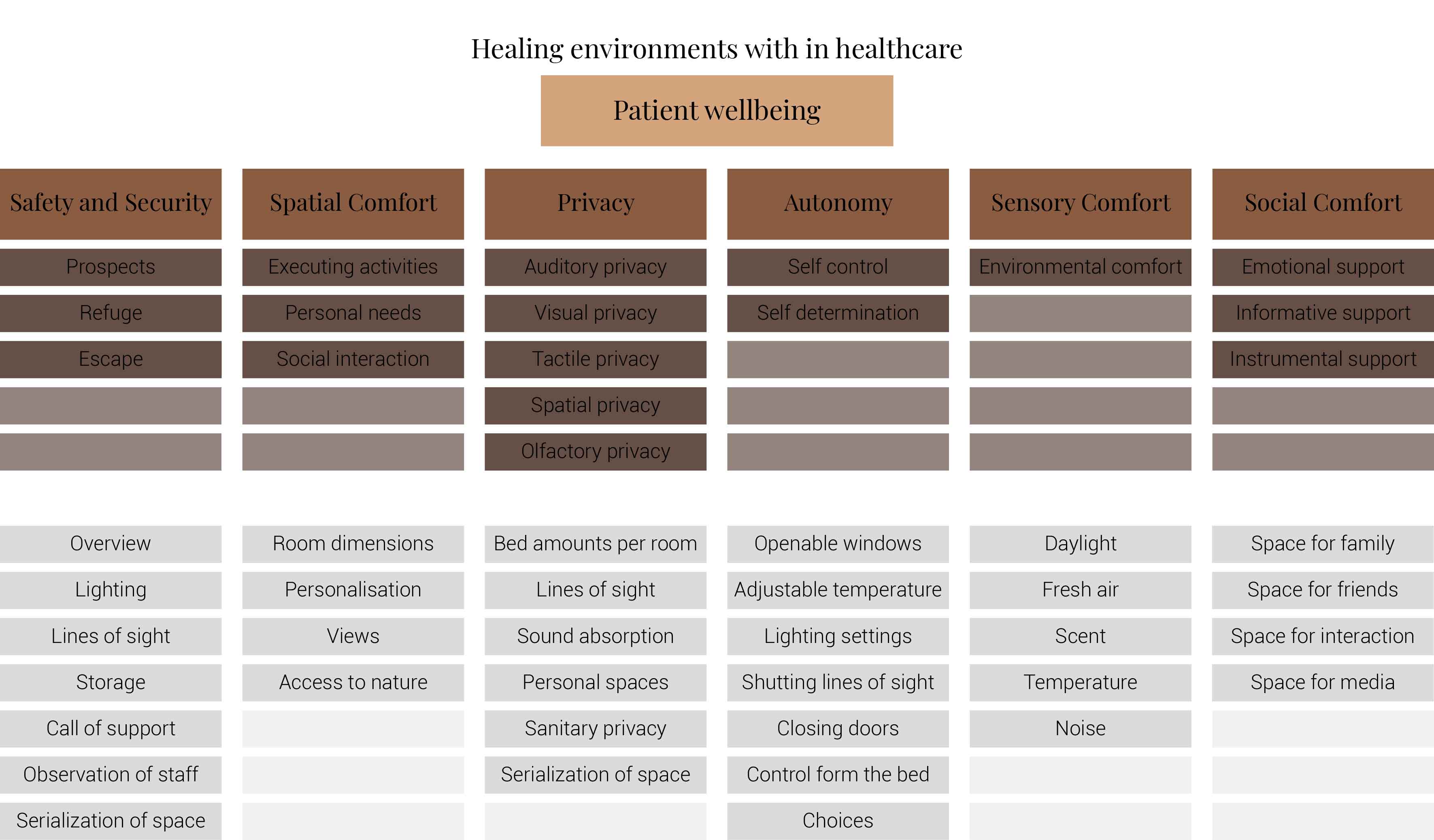
A summary of design characteristics based on the six themes
This image is based on (Schreuder, Lebesque, & Bottenheft, 2016)
The purpose of the research was to find out which design characteristics are more important to the patients than others. Concluding with an advice on which factors should be paid with more attention. It has founded that if hospitals would be transformed into healing environments they should focus on the spatial comfort, safety and security, autonomy and their associated design characteristics.
For spatial comfort it would mean that rooms should be large. It should provide views with sky and green, appealing materials, personal storage space, and space for private conversations.
When it comes to safety and security within the hospital patients appreciate a clear transition form public to private, where unauthorized persons will have restricted access to certain areas. Within the rooms focus should be on lighting, safe personal storage and the ability to call personnel from the rooms.
Many of these characteristics already show some form of autonomy. Another important factor is for patients to have their own influence on what food and drinks the patients consume.But also the possibility to determine resting periods, indoor climate settings and inclusion with decision for treatment.(Schreuder, Lebesque, & Bottenheft, 2016)
While designing all the six themes matter and all their corresponding design characteristics but these previously mentioned characteristics should be integrated with larger importance.
The future of healthcare and the hospital
Healthcare is rapidly changing. This change is fueled by the availability of technology. This change is supported by two interdependent factors.
1. Decentralization.
2. Connectivity.
Challenges that pressure the current healthcare systems.
1. Managing the ubiquity of chronic illness.
2. Caring for an increasingly aging population.
3. The increasing cost of labour.
4. The adoption of new medical technologies.
Two common strategies to help address the growing strains on existing health systems.
1. Community-based healthcare.
2. Connected healthcare.
Shifting left: moving toward community-based healthcare.
Healthcare systems are shifting toward a more patient-centric care in comperrisson to the current situation where the patient will have to go to the care. This shift will result in new settings that could in setting like a patient's home, community health center, schools or workplaces, and many more locations convenient to citizens. But it could also take shape into mobile units that will move around the community.
Besides delivering care within the community, healthcare will start to provide services in the community that can affect health. Research has shown that social and environmental factors can effect a person's health and wellbeing. As a result of the increased person's health and wellbeing the need for healthcare downstream.
The shift left will have various benefits for not just patients but also providers and the health system itself that include the following:
Increased patient comfort and ease.
Individuals that visit a doctor of hospital often suffer from anxiety and discomfort. This can have negative influences on someones wellbeing. With the usage of new technology healthcare could be provided within a more informal setting to put patients more at ease.
More convenience and greater sense of independence and control.
With new technologies and alternative caregiving, patients could be able to manage their own health in collaboration with healthcare specialists. In this way individuals could increase their independences and control.
Better models for managing chronic conditions.
Community care is a more logical approach for chronic disease management and self-management because it allows for more continuous interventionsThere is a growing body of evidence that supports the positive impact of integrating traditional and community-based healthcare for management of integrating traditional and community-based healthcare for management of chronic conditions such as diabetes, hypertension, obesity and frailty in the elderly.
Improved health outcomes.
Researchers have studied community care and its integration with existing formal care resources, and have determined that, generally speaking, patients fare better when cared for outside of institutions (under non-acute conditions). Programs leveraging community-based care have been shown to help patients with congestive heart failure, asthma, diabetes and other conditions to reduce hospital readmissions/emergency visits, improve quality of life, decrease HbA and achieve other positive improvements to their health.
More compassionate end-of-life-care
Currently, most terminally ill and elderly patients pass away in a hospital. It would be much more compassionate to provide end-of-life care at home or in the community, which the majority of these patients have expressed as the preferred setting for their final moments.
Increased focus on prevention and proactive care.
Community care is often focused on early intervention in order to keep the population healthy. This may mean primary prevention (stopping you from getting sick in the first place) or secondary prevention (stopping chronic diseases from advancing to devastating complications).
Challenges.
Existing hospital- and physician-centric paradigm.
Current healthcare initiative usually take place within medical facilities, and the role of physicians is greatly emphasized. But it should revolve around patients. Within healthcare patients are the most important players. Therefor the system should be organized to meet demands of patients instead.
Complexity of care co-ordination.
To ensure that patients receive optimal care an integrated approach towards care is needed. This care co-ordination will depend upon the use of electronic medical records, electronic health record, secure communication tools and other technologies and will require protocols allowing the sharing of personal health information between provides within a patient's circle of care.
Availability of relevant and timely health information.
Healthcare is about communicating information and acting on that information. Therefor it is important to integrate data and communicate findings efficiently. This becomes more complex with concerns about data privacy and security. These factors should also be implemented into the work flow of caretakers and future technologies. Interoperability is key.
Connected healthcare
Achieving a connected healthcare ecosystem
The digitalization and connectedness of health system data is a major priority for health systems around the world. There are three key elements required to ensure access, collection and sharing of information across parties:
1. Electronic medical records (EMRS)
2. Consumer involvement
3. Data & analytics.
1. Role of electronic medical records in connected health.
A core system-level asset in connected health is the electronic medical record (EMR) maintained by healthcare providers, which allows primary care providers to capture and store patient information. Data elements within an EMR can include patient demographic information, diagnosis, lab results, medication, medical history and many others. Supporting solutions include clinical decision support systems (CDSS), computerized physicin order entry (CPOE), and specialized systems, such as picture archiving and communication system (PACS) for storage and access of medical images, and laboratory information management systems (LIMS) for use in laboratory settings. Health information exchanges (HIEs) or repositories bring together the plethora of provider-based digital health data sets to allow ubiquitous access to health information from different vendors, providers and sometimes patients, often across different locations. For HIEs to be effective, the software must follow specific standards that enable the communication between the constituent pieces of software.
2. Role of the consumer in connected health.
From the perspective of the citizen, the building blocks of connected health include digital health technologies such as:
Personal health records (PHRs)
Patient portals
Mobile health and medical apps
Communication tools and social networks
Wearable technologies and sensors
These consumer digital health technologies consist of tools used outside of traditional medical settings, leveraging data found in the formal healthcare system (for example. in the EMR), to increase engagement with a person's circle of care, in order to better track and manage their health. These technologies also carry the potential to redefine how a patient's formal healthcare team can seamlessly keep abreast of their patient's health status, and work together proactively to keep them healthy. For example, in the near future, the concept of scheduling an annual check-up will be outdated.
3. Data and data analytics become central figures in a connected health paradigm.
Digitized medical data is a tremendous asset and vital currency for connected healtcare. With the onslaught of new consumer digital health tools and devices, there is now an abundance of unstructured, patient-generated health data available, in addition to existing, more structured health-related data. This includes health history, lifestyle choices and other information-created, recorded, gathered, or inferred by or from patients or their designees (that is, care partners or those who assist them) to help address a health concern. Further still, a flood of other molecular, genomic, environmental, behavioural and social/contextual data is more available and accessible than ever before. When combined, these data sets form the basis of "Big Data" in healthcare, so called not only for its sheer volume but also for its complexity, diversity and the speed at which it grows. Data analytics brings it all together, completing the connected health ecosystem. Analytics, and the applications that make the data actionable, will ultimately transform healthcare by enabling decisions to be made by each of the members in the full circle of care around an individual.(MacIntosh, 2015)
Smaller and more complex hospitals.
Leading hospitals will be expected to focus on high-value and highly complex services and to become highly efficient organizations, without requiring high activity volumes. Noncomplex services will be shifted from leading hospitals to other healthcare providers, which should provide these routine care interventions at lower costs with a workforce mix and technologies that represent a lower average cost than at the leading hospitals. Leading hospitals will become less capacity-based and more results-oriented as organizations, implementing process improvement to reduce waste and increase value to patients and payers. They will share results and best practices, generating benchmarks for other healthcare providers.
New scope of services.
Leading hospitals will embrace new services such as personalized medicine and genome-based diagnosis, with a broader scope of services.
Leading hospitals will provide complex services to referred patients and also manage the provision of acute services in a catchment area.
Leading hospitals will not be defined by the physical structures and will be organized so they deliver services at different locations. Leading hospitals will adjust to become smaller in terms of physical resources due to fewer inpatient processes, smaller equipment and fewer patients on-site. Leading hospitals will reduce their physical resources on the main site, such as ward areas, and will use distributed facilities to get closer geographically to patients, with processes covering not only on-site activities but also home care and providing services at facilities shared with other levels of care. The size of wards, rehabilitation areas and A&E departments will be adapted to new flows of patients, and resources will be more flexible (suitable for different uses) rather than for a fixed purpose or specialty. In combination, the leading hospital will deliver care at different locations with virtual and flexible, multidisciplinary and process-oriented teams.
Integrated care and process-oriented teams.
Leading hospitals will be organized into process-oriented teams and seek to create integrated care models (either virtually or merging companies). The design of the hospital organization will consider the whole network of provision structuring disease or process-oriented teams, the scope of which extends beyond the hospital facilities. The hospital's role will be not only coordinating but orchestrating services. In order to do that, hospital professionals will share clinical knowledge with other levels of care and providers in the network. Hospital physicians and managers will consider the whole healthcare provision network as their area of influence and will develop and will develop an active role for the care management and improvement, not only within the hospital but also for other providers in the network. In order to manage this healthcare network efficiently. leading hospitals will push forward integrated care models to create either a single integrated care organization (merging entities) or a virtual integrated care organization (a multiple entity organization with a joint governance body).
Connected hospital.
Improvement of the patient experience will lead to connected hospitals where case managers will reach out to coordinate care for patients at home. In the next 15 years, patients will spend less time at hospital and on healthcare premises. Improving the patient experience will demand the introduction between patients and hospital professionals. Information technologies will be used to predict needs, personalize healthcare processes and treatments and follow up and connect with patients wherever they are, using virtual consultation, not only one-to-one but also between a team and patient. Hospital professionals will also become mediators of relevant and personalized information to patients. As remote health management services will become widespread, citizens will use mobile apps, sensors, medical devices to monitor and improve their health and well-being. there will be a wide range of such devices and apps, covering different age and socioeconomic groups in the population almost equally, though there will be different levels of adoption depending on each patient's willingness to communicate remotely and receive directions, support and monitoring. These patients taking a more active role in the design of hospital services and participating in activities to redesign care processes sos patients' needs and views are considered.
Patient-centered innovation.
Leading hospitals will systematically redesign the service experience with innovation to become really patient centered. Hospital services will need to evolve along with clinical knowledge and also with clinical knowledge and also with patient's expectations, systematically evaluating and improving patients' experience and quality of services. Leading hospitals' innovation will promote the establishment of collaborations with other healthcare providers and industry to discover, ideate and prototype new services and new ways of providing services to patients. Patients' involvement in the redesign of healthcare services will be promoted and their perceptions of health services will be consistently evaluated for quality improvement. Innovation activities will not be limited to a small group of practitioners but will extend to most healthcare professionals, and skills and competencies in innovation will be included in the curriculum of different professional career plans.(Ribera, Antoja, Rosenmöller, & Borrás, 2016).
Scenario 3: The downsizing and redeployment of healthcare accelerates the functional deconstruction of the hospital. Care will be widely dispersed across an increasing number of small-scale michohospitals and clinics guided bt smart growth planning principles.
By 2050, a higher number of smaller inpatient care facilities will be dispersed across the landscape; these places will continue to be required in the service of an increasingly acute patient population. Specializations will be more decentralized with few amounts of beds but every room will be acuity adaptable.
Scenario 4: By 2050, the home, not the hospital. will become the center of the healthcare universe. Health promotion (sickness prevention) will be inhibited only by global discrepancies between high-tech versus low-tech societies and the lacuna separating rich from poor.
inequitable acces, combined with the poor quality of healthcare for the poor and disenfranchised, will reach epidemic levels on an increasingly overpopulated planet. A network of microhospitals, as mentioned, will continu to be essential to care only for the sickest of the sick - the most acutely ill.Places other than microhospitals and the neighborhood clinic will have become the epicenter of the healthcare landschape. The patient and familiy (if resources and politics permit) will have universal acces to health information anywhere, anytime. Our home will become a virual clinic. Holograms and microimplants will monitor our health. Holographic consult sessions with your caregiver will occur in the privacy of the family room or kitchen at home.
Dagcentrum Volwassenen (verpleegafdeling)
Dagcentrum Psychiatrie
Dermatologie
Diëtetiek (polikliniek)
Endoscopie (polikliniek)
Geneesmiddelenpoli
Geriatrie
Gipskamer
Types of health.
Healthy
Health at risk/worried well
Unwell/sick
Chronically unwell
Palliative(end of life)
Future developments in healthcare
There is a lot of research and innovation being done in the field of medicine and healthcare. As a species we try to survive as long as possible on this planet. Globally many breakthroughs are being made to improve human health. With innovation not slowing down any time soon it is worth the investigation of what the future developments in healthcare and medicine will be. Below is a video visualising research done by the Economist showing what the future of healthcare and medicine will look like. In my opinion there are seven elements which are very important for healthcare and medicine, these are:
1. Data collection and exchange.
2. Virtual and augmented reality.
3. AI solutions for medication.
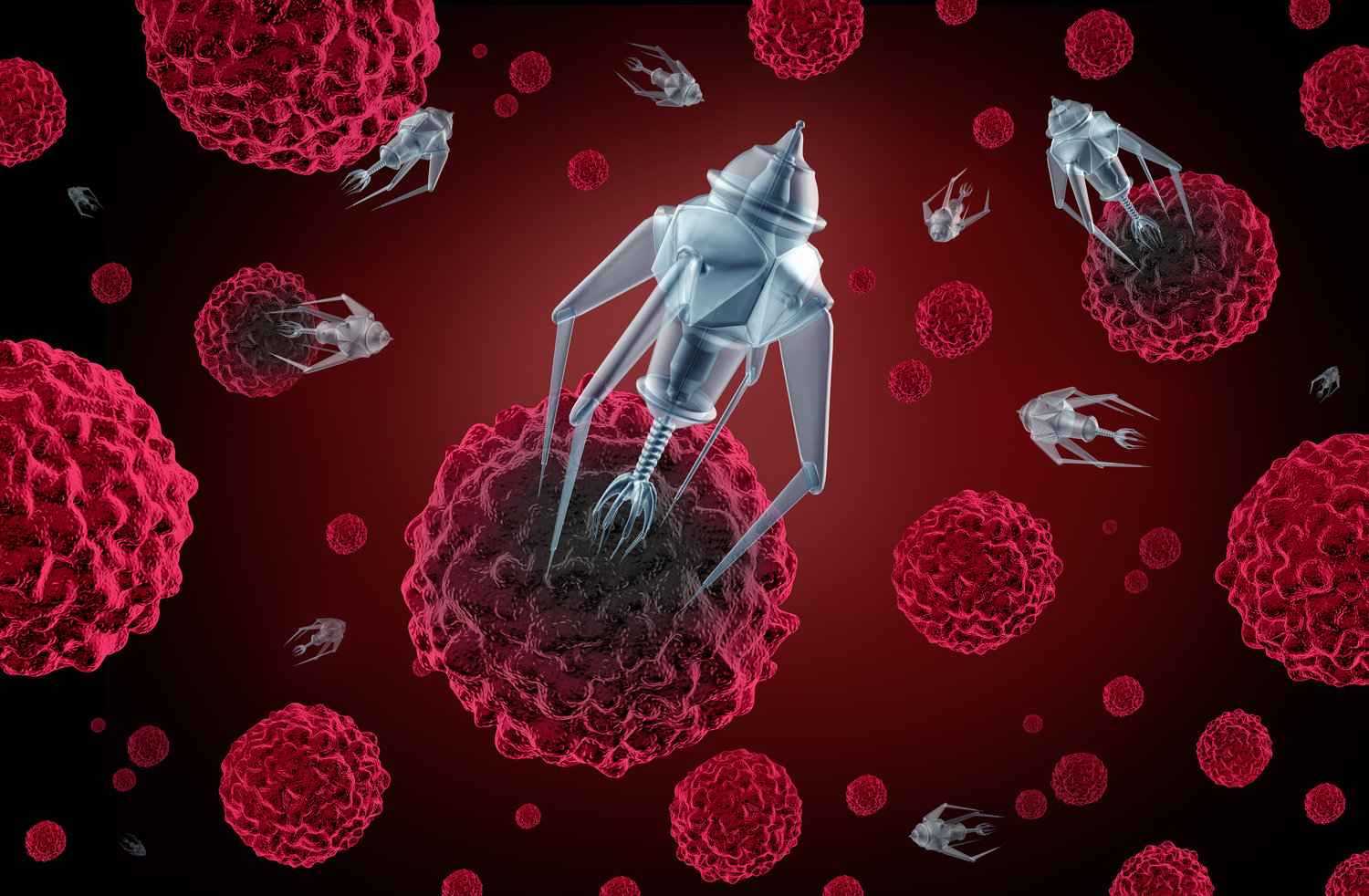
4. Nanomachinery.
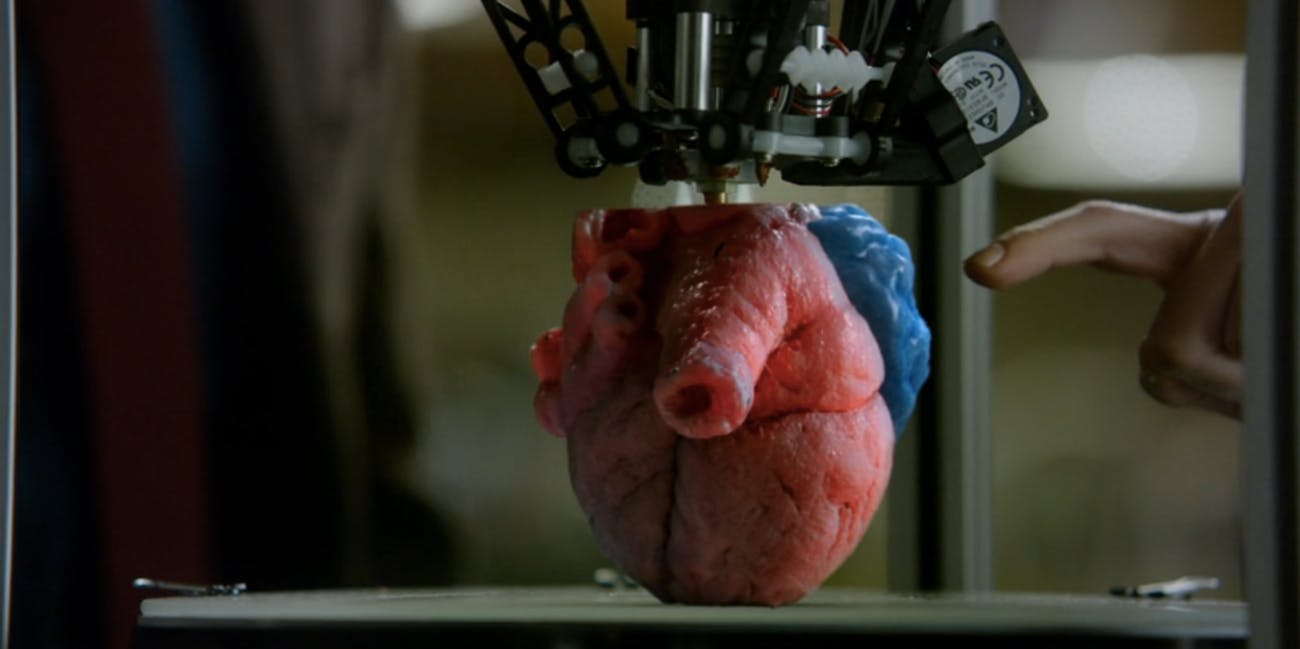
5. 3d printed organs.
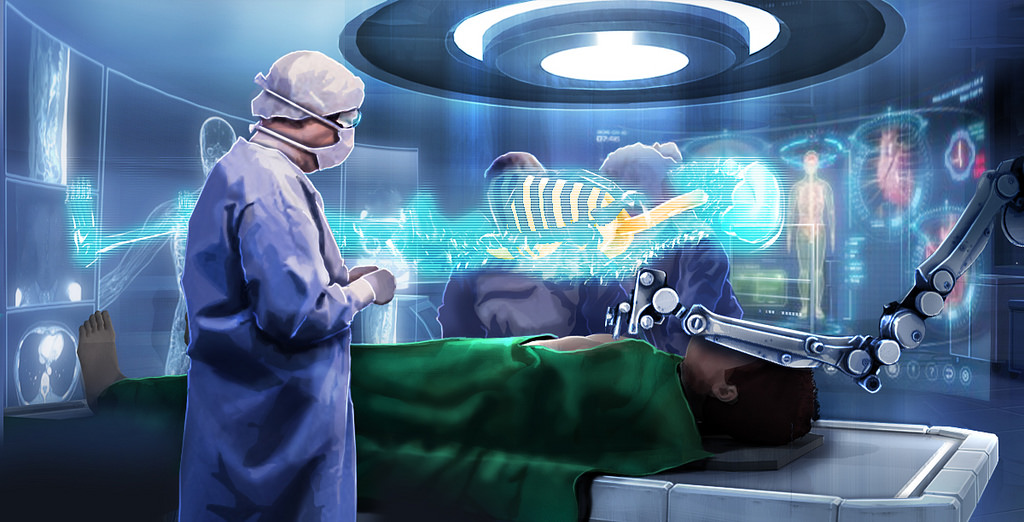
6. Surgery through machinery.
7. Genetical adeption of babies.
A video from the economist portaying the future of healthcare.
A slideshow portaying seven key elements of the future of healthcare.
The Academic Medical Center
The Academic Medical Center